Cardio And Vascular Services
PROFESSIONAL CARDIO SERVICES
Taking care of your heart’s overall health is what we do best at Sam Houston Heart & Vascular Center.
Our facilities in Houston, are fully equipped to provide various cardio services from basic testing to advanced care.
Whether you require diagnostics or surgical treatments, our cardiologist is here to help.
We are dedicated to aiding you in achieving optimum wellness and peace of mind.
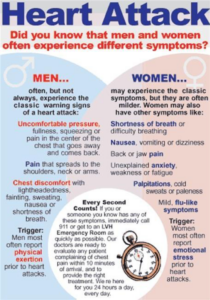
SIGNS OF A HEART ATTACK
- Pain or discomfort – a feeling of heavy pressure, squeezing or burning of the chest, back, neck, arms, jaw, or shoulders
- Unusual shortness of breath
- Weakness, dizziness, or fainting associated with the pain or discomfort as described above
- Excessive sweating, nausea, or vomiting associated with above mentioned symptoms
- Rapid or irregular heartbeat
- A vague feeling of anxiety
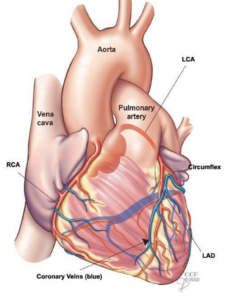
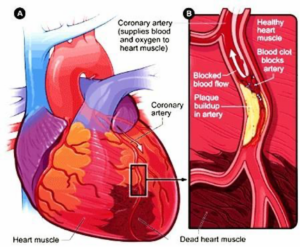
CORONARY ARTERY DISEASE
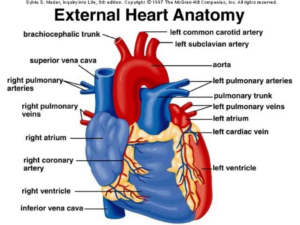
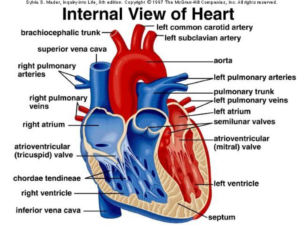
Your heart is a strong muscular pump that is responsible for moving about 3,000 gallons of blood through your body every day. Like other muscles, your heart requires a continuous supply of blood to work properly.
Your heart muscle gets the blood it needs to do its job from the coronary arteries.
What is Coronary Artery Disease?
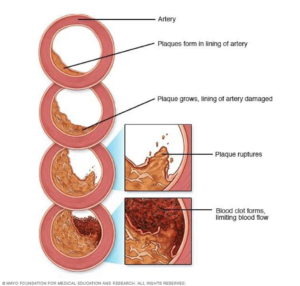
Coronary Artery Disease or CAD, is the narrowing or blockage of the coronary arteries, usually caused by atherosclerosis. Atherosclerosis (sometimes called “hardening” or “clogging” of the arteries) is the buildup of cholesterol and fatty deposits, called plaques on the inner walls of the arteries. These plaques can restrict blood flow to the heart muscle by physically clogging the artery or by causing abnormal artery tone and function.
Without an adequate blood supply, the heart becomes starved of oxygen and the vital nutrients it needs to work properly. This can cause chest pain called angina. If blood supply to a portion of the heart muscle is cut off entirely, or if the energy demands of the heart become much greater than it’s blood supply, a heart attack (injury to the heart muscle) may occur.
DIAGNOSIS AND TREATMENT OF CAD
HOW IS CAD DIAGNOSED?
Depending on your cardiac risk factors and current symptoms, any number of the following testing will be preformed:
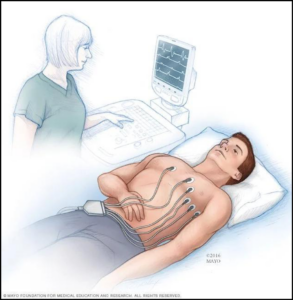
Electrocardiogram
An electrocardiogram records the electrical signals in your heart. It’s a common test used to detect heart problems and monitor the heart’s status in many situations. Electrocardiograms — also called ECGs or EKGs — are often done in a doctor’s office, a clinic or a hospital room. An ECG is a noninvasive, painless test with quick results. During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes your limbs. These sensors are usually left on for just a few minutes.
Each beat of your heart is triggered by an electrical impulse normally generated from special cells in the upper right chamber of your heart (pacemaker cells). An electrocardiogram records the timing and strength of these signals as they travel through your heart.
An electrocardiogram is also called a 12-lead EKG or 12-lead ECG because it gathers information from 12 different areas of the heart. These views are created by electrodes, typically 10, placed on the skin of your chest and sometimes your limbs. The electrical activity is recorded as waves on a graph, with different patterns corresponding to each electrical phase of your heartbeat.
A standard ECG can record an abnormal heart rhythm only if it happens during the test. Some abnormal heart rhythms come and go, so your doctor may have you undergo a different type of heart rhythm monitoring, such as with a Holter monitor, to help diagnose the cause of your symptoms.
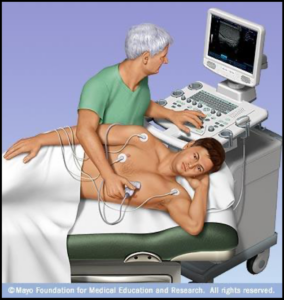
Echocardiogram
An echocardiogram (echo) is a test that uses high frequency sound waves (ultrasound) to make pictures of your heart. The test is also called echocardiography or diagnostic cardiac ultrasound.
An echo uses sound waves to create pictures of your heart’s chambers, valves, walls and the blood vessels (aorta, arteries, veins) attached to your heart.
A probe called a transducer is passed over your chest. The probe produces sound waves that bounce off your heart and “echo” back to the probe. These waves are changed into pictures viewed on a video monitor. Your doctor may use an echo test to look at your heart’s structure and check how well your heart functions.
The test helps your doctor find out:
- The size and shape of your heart, and the size, thickness and movement of your heart’s walls.
- How your heart moves.
- The heart’s pumping strength.
- If the heart valves are working correctly.
- If blood is leaking backwards through your heart valves (regurgitation).
- If the heart valves are too narrow (stenosis).
- If there is a tumor or infectious growth around your heart valves.
The test also will help your doctor find out if there are:
- Problems with the outer lining of your heart (the pericardium).
- Problems with the large blood vessels that enter and leave the heart.
- Blood clots in the chambers of your heart.
- Abnormal holes between the chambers of the heart.
Stress Test
A stress test, also called an exercise stress test, shows how your heart works during physical activity. Because exercise makes your heart pump harder and faster, an exercise stress test can reveal problems with blood flow within your heart.
A stress test usually involves walking on a treadmill or riding a stationary bike your heart rhythm, blood pressure and breathing are monitored. Or you’ll receive a drug that mimics the effects of exercise.
Myocardial perfusion scan with pharmacologic intervention Your doctor may recommend a stress test if you have signs or symptoms of coronary artery disease or an irregular heart rhythm (arrhythmia). The test may also guide treatment decisions, measure the effectiveness of treatment or determine the severity if you’ve already been diagnosed with a heart condition.
In our office we preform 3 types for stress test: regular treadmill stress test, Myocardial perfusion scan with exercise, and Myocardial perfusion scan with pharmacologic intervention.
WHAT IS A STRESS MYOCARDIAL PERFUSION SCAN?
A myocardial perfusion scan is a type of nuclear medicine procedure. This means that a tiny amount of a radioactive substance, called a radionuclide (radiopharmaceutical or radioactive tracer), is used during the procedure to assist in the examination of the tissue under study. Specifically, the myocardial perfusion scan evaluates the heart’s function and blood flow.
A radionuclide is a radioactive substance used as a “tracer,” which means it travels through the blood stream and is taken up (absorbed) by the healthy heart muscle tissue. On the scan, the areas where the radionuclide has been absorbed will show up differently than the areas that do not absorb it (due to possible damage to the tissue from decreased or blocked blood flow).
A stress myocardial perfusion scan is used to assess the blood flow to the heart muscle (myocardium) when it is stressed by exercise or medication and to determine what areas of the myocardium have decreased blood flow. This is done by injecting a radionuclide (thallium or technetium) into a vein in the arm or hand.
There are different types of radionuclides. When one type of radionuclide is used, areas of the myocardium that have blocked or partially blocked arteries will be seen on the scan as “cold spots,” or “defects,” because these areas will be unable to take in the radionuclide into the myocardium. Another type of radionuclide binds to the calcium that is released when a heart attack occurs, so it will accumulate in area(s) of injured heart tissue as a “hot spot” on the scan.
There are two types of stress myocardial perfusion scans, one that is used in conjunction with exercise (myocardial perfusion scan with exercise) and one that is used in conjunction with medication (pharmacologic myocardial perfusion scan).
Myocardial perfusion scan with exercise
A myocardial perfusion scan with exercise is used to determine what areas of the heart muscle (myocardium) demonstrate decreased blood flow during exercise. This is done by injecting a radionuclide (thallium or technetium) into a vein in the arm or hand during exercise. After the radionuclide has been injected into a vein and has circulated through the blood stream, a special machine called a gamma camera takes pictures of the heart while the person lies still on a table. This scanning usually lasts about 30 minutes.
Any areas of the myocardium that have blocked or partially blocked arteries during exercise will be seen on the scan as “cold spots,” or “defects,” because these areas will be unable to absorb the radionuclide into the myocardium.
A second set of scans is taken some hours later, at rest. The resting phase is done in order to compare the results with the exercise phase to see if areas that do not get adequate blood flow while exercising are able to absorb the radionuclide during rest.
Myocardial perfusion scan with pharmacologic intervention
A pharmacologic myocardial perfusion scan is used when the physician has determined that exercise on a treadmill is not an appropriate choice due to the person’s medical condition. In this situation, a medication is given that causes the coronary arteries to dilate. This dilation of the coronary arteries increases blood flow and is very similar to the response of the arteries during exercise. The medication is injected into a vein in the arm or hand.
After a given period of time, the radionuclide will be injected into a vein in the arm or hand. The gamma camera will take pictures of the heart while the person lies still on a table. A resting scan will be performed afterwards, just as with the actual exercise scan.


CORONARY ANGIOGRAM OR LEFT HEART CATHETERIZATION
Coronary angiography is a procedure that uses contrast dye, usually containing iodine, and x ray pictures to detect blockages in the coronary arteries that are caused by plaque buildup. Blockages prevent your heart from getting oxygen and important nutrients. This procedure is used to diagnose coronary heart disease and coronary microvascular disease after chest pain, sudden cardiac arrest, or abnormal results from tests such as an electrocardiogram (EKG) of the heart or an exercise stress test. It is important to detect blockages because over time they can cause chest pain, especially with physical activity or stress, or a heart attack. If you are having a heart attack, coronary angiography can help your doctors plan your treatment.
You will stay awake so you can follow your doctor’s instructions, but you will get medicine to relax you during the procedure. You will lie on your back on a movable table. Often, coronary angiography is done with a cardiac catheterization procedure. For this, your doctor will clean and numb an area on the arm, groin or upper thigh, or neck before making a small hole in a blood vessel. Your doctor will insert a catheter tube into your blood vessel. Your doctor will take x ray pictures to help place the catheter in your coronary artery. After the catheter is in place, your doctor will inject the contrast dye through the catheter to highlight blockages and will take x ray pictures of your heart. If blockages are detected, your doctor may use percutaneous coronary intervention, also known as coronary angioplasty, to improve blood flow to your heart.
After coronary angiography, your doctor will remove the catheter, possibly use a closure device to close the blood vessel, and close and bandage the opening on your arm, groin, or neck. You may develop a bruise and soreness where the catheter was inserted. You will stay in the hospital for a few hours or overnight. During this time, your heart rate and blood pressure will be monitored. Your movement will be limited to prevent bleeding from the hole where the catheter was inserted. You will need a ride home after the procedure because of the medicines or anesthesia you received.
After coronary angiography, your doctor will remove the catheter, possibly use a closure device to close the blood vessel, and close and bandage the opening on your arm, groin, or neck. You may develop a bruise and soreness where the catheter was inserted. You will stay in the hospital for a few hours or overnight. During this time, your heart rate and blood pressure will be monitored. Your movement will be limited to prevent bleeding from the hole where the catheter was inserted. You will need a ride home after the procedure because of the medicines or anesthesia you received.
AFTER THE PROCEDURE
Discharge Instructions Post Angiogram/Cardiac Catheterization
Dressing:
If the band aid was not removed in the hospital, you may remove it once you get home, unless otherwise instructed. It is less painful if you need to remove it while in the shower.
Bathing:
You may shower the day after the procedure. Gently cleanse the site with soap and water 24 hours after the procedure. You may not take a bath, swim or soak in a hot tub or Jacuzzi until after your office follow up appointment.
Exercise:
You may resume walking at home. After 24 Hours, you may walk the distance at which you are accustomed. If you have not been walking, you may start at a low level. If you procedure was performed via your radial artery (wrist): DO NOT hyperextend your wrist for 7 days.
Sexual Activity:
You may resume after 48 hours, unless advised otherwise.
Household Chores:
You may resume household chores (dishes/laundry).
Lifting:
Femoral artery approach (leg/groin): DO NOT lift over 10 pounds for first 3 days at home. Radial or Brachial artery approach (wrist/arm): DO NOT lift over 7 pounds with the affected arm for 7 days.
Driving:
You may resume 24 hours after discharge, unless advised otherwise.
Stairs:
As Tolerated
Work:
Depends on your type of work. Check with your Doctor.
Medications:
Take as directed. DO NOT stop any medications unless you are instructed by your cardiologist. Contact the office for specific instructions.
Diet:
Follow a low fat, low cholesterol, heart healthy diet. If you have any other dietary restrictions, follow your doctors recommendation.
Smoking:
Smoking is a major risk factor for most diseases. If you smoke, your are strongly encouraged to quit. Talk to your Doctor for assistance.
Notify your Doctor If:
Chest pain (angina) returns. Take Nitroglycerin as directed. Temperature higher than 101.5. Bleeding at the puncture site. Femoral artery approach (leg/groin): Leg is white, numb, cold, very painful, or if a lump appears at the incision site. Radial or Brachial Artery Approach (wrist/arm): arm is white, numb, cold, very, painful, or if a lump appears at the incision site.
Follow-Up Appointments:
Schedule and Keep your appointment for 7-10 days post procedure. Your Cardiologist will check your puncture site at this appointment.
CARDIAC REHABILITATION
What Does Cardiac Rehab Involve?
Cardiac rehab doesn’t change your past, but it can help you improve your heart’s future. It’s a medically supervised program designed to help improve your cardiovascular health if you have experienced heart attack, heart failure, angioplasty or heart surgery. Think of cardiac rehab as three equally important parts:
- Exercise counseling and training: gets your heart pumping and your entire cardiovascular system working. You’ll learn how to get your body moving in ways that promote heart health.
- Education for heart-healthy living: Managing risk factors, choosing good nutrition, quitting smoking…education about heart-healthy living is a key element of cardiac rehab.
- Counseling to reduce stress: Stress hurts your heart. This part of rehab helps you identify and tackle everyday sources of stress.
Cardiac Rehab is a Team Effort
You don’t need to face heart disease alone. Cardiac rehab is a team effort. It’s a medically-supervised program in which you partner with your doctors, nurses, pharmacists — plus family and friends — to take charge of the choices, lifestyle and habits that affect your heart.
What’s Next?
You’re in the driver’s seat…but here’s what we suggest to get started:
- Ask your doctor if you are eligible for cardiac rehab.
- If you are eligible for cardiac rehab, register for a program.
- In consultation with your medical team, set some heart-health goals and create a cardiac rehab plan.
- Take an active role in your care to achieve your goals.
- Keep taking your medicines correctly.
- Call 911 if you experience new or worsening symptoms.
CONSULT OUR CARDIOLOGIST
Learn the best care and treatments for various cardio problems by turning to the specialists of Sam Houston Heart & Vascular Center. Our doctors are knowledgeable and experienced in analyzing heart diseases and providing treatments for different health issues concerning the human heart. Aside from cardio services, we also provide vascular treatments for your added convenience. Should you have any questions about what we do, call or email us using the provided contact details. We look forward to serving you soon.
OUR CARDIO SERVICES
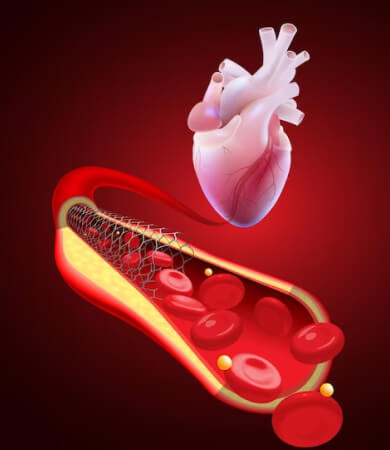
- Angioplasty (PTCA) and Coronary Stent
- Echocardiogram
- Electrocardiogram
- Event Monitor
- Exercise Electrocardiogram (Treadmill Stress Test)
- Holter Monitor
- Pacemaker/Implantable Cardioverter Defibrillator (ICD) Insertion
- Stress Myocardial Perfusion Scan (Nuclear Stress Test)
- Vascular Studies